Cleanrooms aren’t as clean as you may think. New research has found multiple taxonomic groups of microbial signatures that escaped detection by conventional, culture-dependent monitoring methods. While these signals reflect relative abundance based on DNA sequencing rather than viable counts, several of the 28 dominant groups—each contributing at least 5% of the detected microbial composition—underscore that previously invisible contaminants can be present even in highly controlled environments.
“The findings highlight the need for complementary monitoring strategies that go beyond colony-forming units and particle counts, and for advancing detection methods capable of identifying risks before therapeutic products reach patients,” Mitsuru Mizuno, PhD, assistant professor, Institute of Science Tokyo, tells GEN.
Mizuno and Institute researchers, along with collaborators at bitBiome, a biotechnology startup based at Waseda University, in cooperation with Takenaka, collected airborne bacterial DNA using a high-volume air sampler from environmental grade B, C, and D cleanrooms, which are areas used for gowning, material introduction, staging, formulation, and buffer prep.
“Grade A cleanrooms [used for aseptic filling and capping operations] were not included in this study, as they are maintained under highly controlled conditions that typically preclude the detection of microbial DNA under normal operation,” Mizuno says. “In our verification, no bacterial nucleic acids were detected in Grade A zones, and therefore these areas were not suitable for evaluating the comparative advantages of microbiome-based monitoring over traditional methods.”
Environmental monitoring techniques
Environmental monitoring methods that rely on particle counts and culture-based colony-forming unit measurements “fail to capture much of the diversity and provenance of airborne microbes,” Mizuno and colleagues wrote. That’s because many microbes either can’t be cultured or won’t grow on standard culture media.
Skin-related bacteria, including Cutibacterium and Corynebacterium, and environmental bacteria, including Bacillus and Paracoccus, were consistently found in each of the cleanrooms, across all grades, the researchers note. They detected skin-related bacteria at irregular intervals, suggesting “operator-related, non-persistent contamination.” Furthermore, the presence of these groups indicates that microbial ingress and colonization are not completely eliminated, even in cleanrooms.
“Overall microbial diversity is not substantially influenced by environmental grade,” they stress. It is, however, influenced heavily by localized airflow patterns, work tasks, and equipment operation that spread microbial communities into adjacent areas. The usual cleanroom zoning strategies, therefore, can be compromised
Contamination in low-mass cleanroom environments is inevitable “when working near the limits of detection,” researchers from the National Aeronautics and Space Administration (NASA) concluded earlier this year.
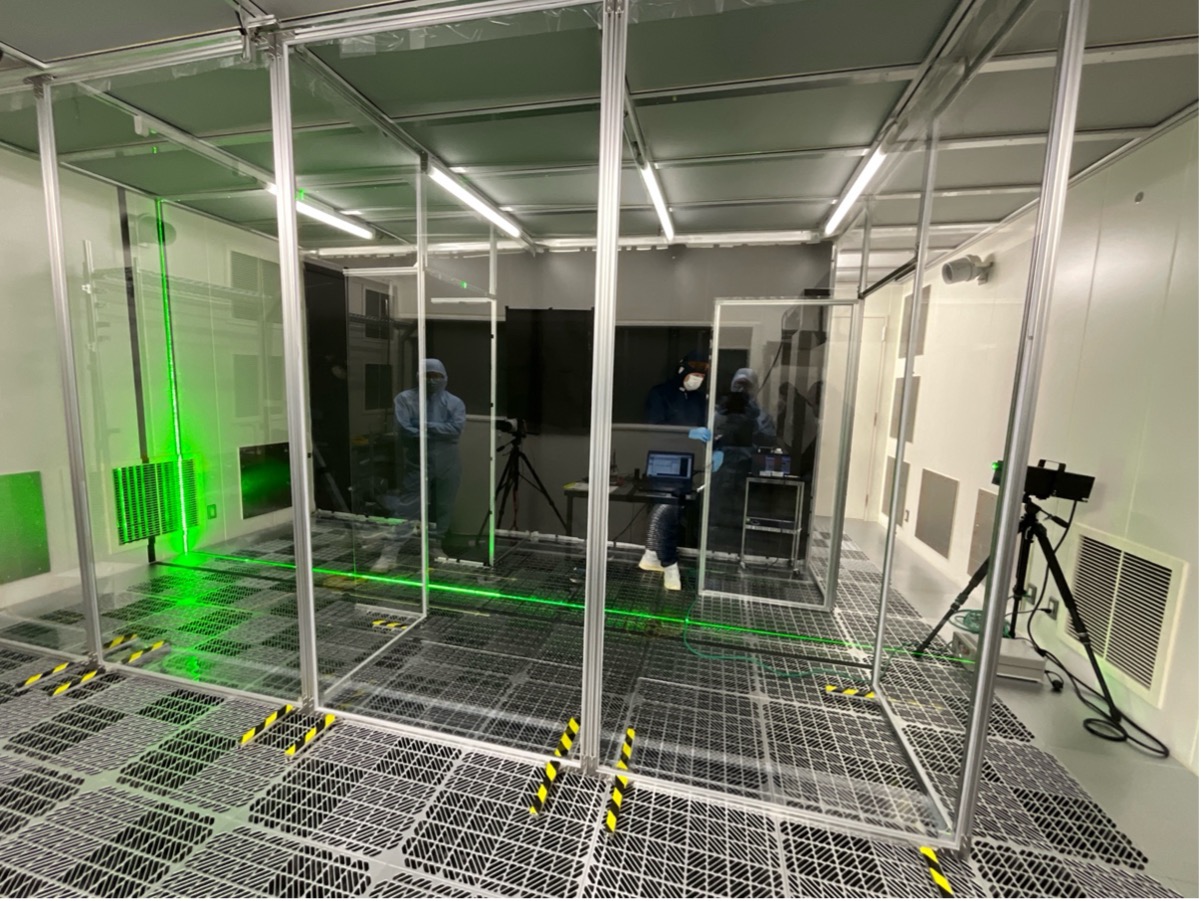
Air-barrier cleanrooms for cell products processing are one possible solution, Mizuno and Takenaka propose. By replacing the doors between the cell processing cleanroom and the corridor with unidirectional air curtains, the team restricted the particle transfer that occurs when operators exit the room to 0.013%. In a simulation, the team estimates that only 0.004% of particles reach the adjacent room. This approach also reduces energy demands and capital costs compared to sealed, multi-room suites, and supports staff mobility.
When considering air-curtain options, Mizuno and colleagues report that push-pull ventilation in this semi-open clean room offers the best containment of contamination that occurs when people walk between rooms. Alternatively, using “supply-air flow to restrict particle transport” and “adding 500 mm (about 20 inches) wing walls offers a passive alternative with moderate protection.”
“Such semi-open, door-free designs not only facilitate energy efficiency and operational flexibility but also open the possibility of incorporating robotic operators into the cleanroom workflow—an attractive option for tasks such as routine environmental monitoring that do not depend on human dexterity,” Mizuno says. “Still, despite the reduced contamination risk achieved through airflow engineering, these designs do not eliminate contamination entirely. Therefore, the development and integration of high-sensitivity detection methods must proceed in parallel to identify residual contaminants before products are administered to patients.”
As Mizuno adds, “Advanced sequencing has enabled detection of microbial species that traditional agar culture methods could not reveal. This does not imply an increase in contamination; rather, it makes long-standing, previously invisible risks more apparent. Because humans are an unavoidable source of contamination in cleanrooms, complete prevention isn’t feasible. Our position is to coexist with such risks while developing and refining sensitive detection.”